
Every healthcare facility uses a different process for credentialing providers, but most face common challenges.
- Getting complete and accurate information from providers
- Communicating with stakeholders, both internal and external
- Completing reviews in a timely manner
Top issues in credentialing locum tenens providers
A recent survey conducted in partnership with the Association for Advancing Physician and Provider Recruitment (AAPPR) identified the top problems experienced by healthcare facilities when credentialing locum tenens physicians.
1. Incomplete or inaccurate paperwork
The number one problem in credentialing locum tenens providers is not receiving everything needed or inaccurate/out-of-date information.
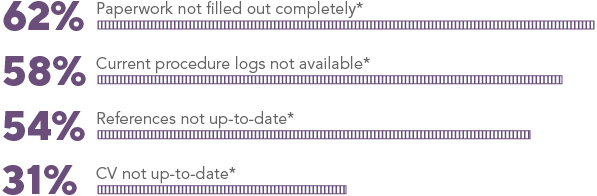
*Percentages shown reflect the number of respondents who stated that this was a problem at least half of the time.
2. Agency interaction
Survey respondents expressed that they are frequently dissatisfied with the quality of their interactions with locum tenens agencies.
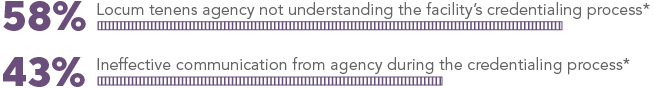
*Percentages shown reflect the number of respondents who are extremely or somewhat dissatisfied.
When the credentialing and recruiting functions are separate at a facility, the problem is more pronounced. Forty-eight percent of teams who are separated by credentialing and recruiting functions had trouble receiving effective communication from the locum tenens agency, compared to 34 percent of teams with a shared reporting structure.
Example: If the recruitment team and an agency negotiate without coordinating with credentialing, it can result in added stress and frustration when credentialing has to accelerate the credentialing timeline in order to meet a promised deadline. Good inter-team communication is the best way to prevent these credentialing issues and ensure alignment on timelines.
3. Job/provider match
A less significant but critically important concern is matching the right provider with the right job. The presentation of unqualified or mismatched providers for openings was identified as a problem for 35 percent of survey respondents.
4. Length of credentialing process
A long credentialing process can be a problem for healthcare facilities, especially when there’s an urgent need for a locums physician.
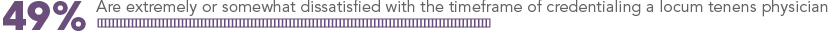
Reducing the timeframe to complete credentialing by even a few days can translate directly into increased ROI for the facility.
8 tips to help make credentialing locum tenens easier and faster
The following practices can help reduce problems and setbacks when credentialing a locum tenens provider.
 1. Agree on the application completion process
1. Agree on the application completion process
Proactively set expectations with the locums agency on how you will work together to complete the application process. What constitutes a completed application can mean different things to different parties. Consensus between your facility, the provider, and the agency is key to timely completion.
Example: The locums agency is still in the process of credentialing Dr. Smith, who has been presented for an open position. Complete information is not yet available when Sharon from the hospital’s credentialing department starts the locum tenens provider credentialing process. Sharon asks her contact at the agency to provide Dr. Smith’s status and when she can expect to get the missing information. She also requests to be notified if anything changes.
 2. Communicate your credentialing process
2. Communicate your credentialing process
Many agencies can assist you in credentialing locum tenens, but they will be more effective if they clearly understand:
How they can and can’t help
- What do your bylaws require?
- What tasks will you allow the agency to perform?
- Is there a credentialing checklist you can share with the agency?
- Can the agency assist in obtaining professional references?
- Can the agency make follow-up calls to help obtain documents and/or primary source verifications?
What your credentialing requirements are
- How do your requirements differ from the agency’s credentialing requirements?
- If they are different, can the agency still help you gather the needed information?
- What do you consider to be concerns or red flags?
What your privileging requirements are
- Do you grant temporary privileges for locum tenens providers?
- If so, what needs to be completed before you can make a decision?
What your expectations are
- How do you want to communicate with the agency and how frequently?
- What are your timelines, meeting dates, and important deadlines? Example: If a provider isn’t licensed to work in your state, when does the license need to be obtained in order to meet your deadlines?
 3. Streamline your process
3. Streamline your process
If it’s a challenge to clearly communicate your process, you may want to consider conducting a formal evaluation to discover opportunities for improvement. Streamlining your process could result in:
- A shorter credentialing timeframe
- Faster review process
- Improved communication with internal and external stakeholders
CompHealth has used a variety of methodologies to improve and streamline our own processes, including the provider credentialing process. Two options that can help you are the kaizen methodology and the Lean methodology.
 4. Ensure a detailed practice description
4. Ensure a detailed practice description
Complete and thorough practice descriptions can help reduce the number of candidate presentations that don’t match the need. A more detailed practice description will better enable the agency to provide you with applicants that match your requirements. Better qualified applicants mean less time on your part filtering out unacceptable candidates during the credentialing process.
 5. Communicate provider expectations early
5. Communicate provider expectations early
If you are communicating with the provider directly, connect your credentialing staff with the provider as early in the process as possible to set expectations and answer questions.
Keep things simple by providing a clear, comprehensive checklist of what they need to do and by when. Make sure they have easy access to any forms and documents they will need.
 6. Watch for red flags
6. Watch for red flags
As soon as you start to receive information about a provider — whether from the agency or the provider directly — begin reviewing their credentials to identify any red flags. Identifying red flags early in the process can save time credentialing candidates who do not meet your requirements.
 7. Fully address all concerns as soon as possible
7. Fully address all concerns as soon as possible
Although they might not be red flags, even minor concerns should be addressed as early as possible. Quick resolution of concerns gives you and the provider confidence to move forward with the credentialing process.
- Investigate: Dig deeper using available resources (Example: You identify a potential health concern. Get a release and discuss with the candidate’s treating physician.)
- Discuss: Bring your concerns to the agency/applicant to ensure a clear understanding
- Manage: Follow up to verify all concerns have been properly addressed/mitigated
 8. Follow up with primary sources
8. Follow up with primary sources
A good way to avoid delays in primary source verification is to proactively follow up. Here are three tips that can help.
- Reach out: Call the facility and ask for the name of the person who receives verification requests. This will help you make sure it gets to the right destination.
- Follow up: Once you have sent the request, follow up to make sure it was received by the correct person, then ask when you can expect a response.
- Understand preferences: Ask how often you should follow up the primary source and what their preferred method of communication is; it will help you avoid becoming a nuisance.
How a good agency can help
An agency can be a help or hindrance in credentialing locum tenens providers. Here’s how a good agency can facilitate the process.
Presenting only qualified candidates who match your need
Agencies work with two kinds of providers:
- Currently credentialed providers
- New providers who are still being credentialed by the agency
A new provider may be presented for jobs where they appear to be the best fit, even though they may not have completed the agency’s credentialing process. Although this presents some risk to both the agency and the facility, it can often result in a positive outcome for everyone. The downside of accepting a candidate of this status is the risk that a problem may arise during credentialing. The upside is the candidate may help you fill the position more quickly.
Tip: If you are willing to consider a provider who hasn’t yet been fully credentialed by the agency, set up a phone interview with the candidate and the appropriate clinical department head. This will allow you vet the candidate early in the process.
Communicating expectations to the candidate
An agency already has a relationship with the provider they are presenting, so they may be able to help by communicating the following to the candidate:
- The timeframe to complete the credentialing process and important milestones that need to be met to stay on track
- All hospital privileging requirements, including required paperwork and clear expectations for turnaround times
- What it means for the paperwork to be completed in full
 Educating their providers
Educating their providers
Many providers leave blanks on an application because they lack needed information. An agency can educate its providers on the importance of keeping all certificates, legal documents, letters, and other documents related to their practice and storing them in a safe, dry place where they won’t degrade. Providers who have been coached on good organizational habits are easier to credential.
Helping with the legwork
A good agency should have an internal team dedicated to the credentialing process. The agency team should provide all applicable and legally shareable documents they have on the candidate in a timely manner. This will help accelerate the process of identifying what is still needed. The agency can also follow up directly with the provider to ensure they’ve completed all paperwork and submitted it in a timely manner.
Helping with the credentialing
Facilities that need more resources dedicated to credentialing may benefit from a delegated credentialing agreement. A delegated agreement allows a healthcare organization to entrust primary source verification to another organization, such as a Credentials Verification Organization (CVO). Delegated credentialing may be able to reduce the time it takes for a provider to be granted privileges at a hospital and speed up the provider enrollment process.
 Pros of a delegated agreement
Pros of a delegated agreement
- An agency can take on the entire credentialing process or provide assistance only on the parts that are challenging or time-consuming for your facility
- Agencies already have a working relationship with applicants and often have many of the records needed for credentialing, which can make it easier to get primary source verifications that meet nationally recognized standards
- Weekly file status reports provided by the agency can make it easy to track applicants and pass information upstream to your leadership team
- Delegated credentialing creates efficiencies and eliminates duplicate effort that can be a burden for the applicant
- Accuracy can be monitored through regular file audits
 Cons of a delegated agreement
Cons of a delegated agreement
- Your facility has less direct control over the credentialing process
- Management could potentially have concerns that delegated credentialing might not be recognized by an accreditation body
If you do chose to delegate to a third party, be sure they are a nationally certified CVO or meet nationally recognized standards.
Communicating well and often with you
The AAPPR survey found that 86 percent of credentialing personnel felt regular process updates are very or extremely important. A good agency will communicate regularly where they are in the credentialing process — both in the agency’s own internal credentialing and in your processes. All parties should receive regular updates on what’s been received and what’s still needed. Open communication is critical to keeping things moving forward.
Communications tip: If you are credentialing multiple providers simultaneously or have multiple people involved in the process, regular conference calls can streamline communications and ensure progress. A shared spreadsheet showing the status of all providers is another good way to communicate status at a glance.
For permanent placements
An agency can also assist with credentialing permanent positions, depending on the facility and its needs. Talk to your agency to learn how they can and can’t help. For example, they may be able to provide information they have already gathered from the provider, but they can’t fill out forms on their behalf.
Additional resources
Although credentialing locum tenens can be challenging, the CompHealth team is always ready to assist you in the process. Give us a call at 800.453.3030 or complete the form below to learn more.
You may also find the following resource helpful: Credentialing Resource Center